IVF Procedure
A 7 Step Process for Making a Baby (Steps 1 & 2)
By Paul J.O'Brien B.A., N.C.E.H.S., Dip. Acu., Adv. Dip. OBB, Cert Clin. Med, Cert.CHM, Pn1, PN-SSR, PN-NCA, M.AFPA, M.ETCMA, M.C.Th.A.
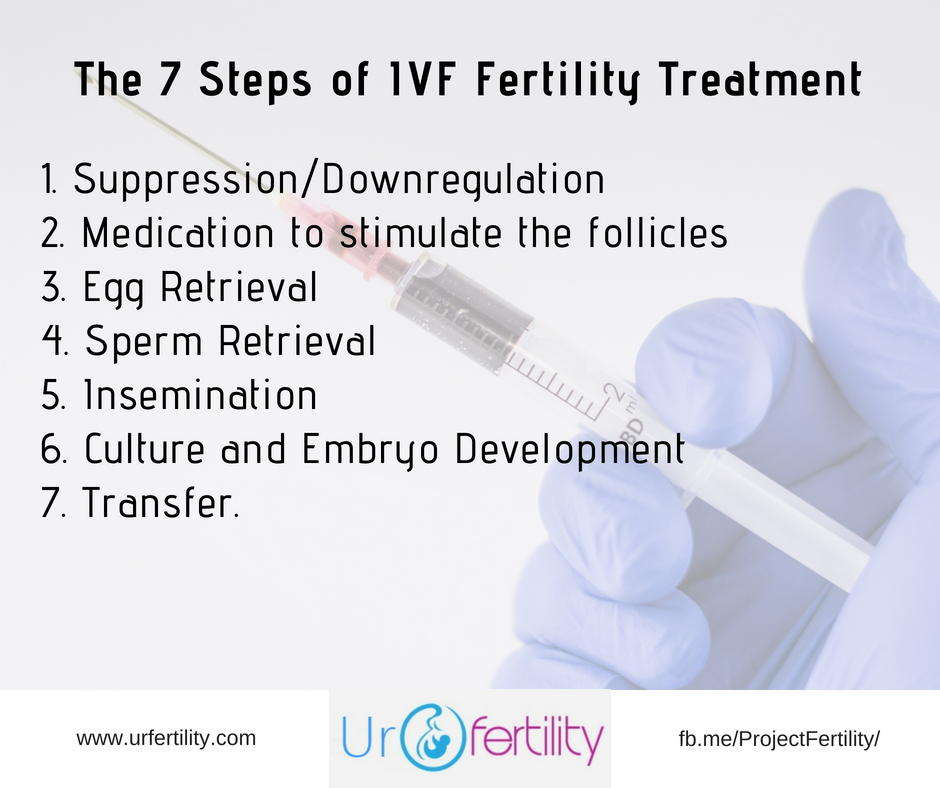
IVF procedure, regardless of the fertility clinic you attend, follows the same basic 7 step format. A format that produces less than optimal results. Worldwide statistics show the avg live birth rate is 20.2%(1). Thankfully I can show you how to do much better using all natural methods, which I’ll cover in a moment.
First though, let’s look at the standard system:
IVF Procedure Step 1: Suppression / Downregulation
This is considered a pre- IVF procedure phase, where a patient will likely be placed on either a Gonadotrophin Releasing Hormone (GnRH) agonist or a GNRH antagonist. This drugs are used to prevent the release of Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH) by the pituitary gland. These are the two hormones used to grow and develop your follicles and eggs (FSH), and the hormone that triggers the release of the egg (LH). The goal here is to prevent a natural ovulation and thus give the body a longer amount of time to build up egg numbers.
The GnRH agonist phase, which is the mostly commonly used in my experience with fertility clinics, can be further divided into a “long protocol” or a “short protocol”.
The long protocol ivf procedure usually starts around the mid luteal phase of the pretreatment cycle (so roughly around the week after ovulation and the week before the period is due), though in some cases can start up to 4 weeks before ovarian stimulation is due to begin. This is a suppression/downregulation phase.
In the short protocol the drugs are taken on day 2 or 3 of the menstrual cycle, once a baseline new uterine lining has formed (2)(3).
Unfortunately both of these protocols of IVF procedure are associated with negative side effects. The long protocol is associated with the development of ovarian cysts, headaches, and hot flushes as well as oestrogen deficiency (a hormone needed to grow and develop the follicles ironically). Both long and short are associated with the risk of the serious medical condition of Ovarian Hyperstimulation Syndrome (OHSS), which can, and has, resulted in patient death (though this is rare)(4).
By contrast the GnRH antagonist protocols has no downregulation. The drugs are taken on day 5 or 6 of the menstrual cycle and instantly shut down the pituitary glands ability to release FSH and LH.
Unfortunately this too is associated with negative side effects. Firstly it is unpredictable, and impossible to schedule or determine when egg retrieval will occur. More concerning however, is that in an attempt to regulate egg retrieval the oral contraceptive pill is usually provided. Studies have shown though that this significantly reduced rates of ongoing pregnancy (5) (6).
IVF Procedure Step 2: Medication
In this second stage of IVF procedure, fertility medications are prescribed to stimulate egg production. These are often injections of Gonadotrophins hormones of FSH and/or LH and range from 150 IU to 450 IU a day. There are three major types of these drugs:
- Urinary extracts: Human Menopausal Gonadotrophins (hMG) (menootrophin) which contain FSH and LH i a 1:1 ratio, with Merional and Menopur being the most common prescriptions.
- Purified urinary extract FSH, the most common of which is Fostimon
- Recombinant synthetic hormone of rFSH, the most common of which is Gonal-F.
A question I am commonly asked is which is better? Truth is, there’s no real difference. A 2011 Cochrane review found there was no difference in effectiveness between the various preparations - so go with the cheapest and easiest available (7).
A transvaginal ultrasound is used to examine the ovaries around days 5-7 of the stimulation stage and repeated every 2-3 days. Additionally blood test samples are taken to check hormone levels.
In a normal cycle a woman will release one dominant egg per month, however for IVF fertility treatment they try to produce a year’s worth of eggs in a single month. It’s essentially a numbers game. The reality is that not every egg will develop or fertilize after retrieval, nor will every embryo survive to transfer.
As such most IVF fertility treatment clinics strive to develop 15 eggs. The study this figure is based on indicated that to produce 1 and 2 euploid embryos (normal chromosomes), 5 and 14 oocytes would be required at age 34. However 10 and 24 oocytes would be required at age 38. This indicates that the older a woman is the more eggs have to be retrieved in order to increase the chance of obtaining an additional chromosomally normal (euploid), healthy, embryo(8).
If the number of eggs rises above 20 per cycle, the clinic will likely cancel the cycle as this high a number can indicate a diminishment of size and quality, but more seriously indicate Ovarian Hyperstimulation Syndrome (OHSS). All that said however, the number of eggs developed is dependant on how many follicles a woman has left, her reaction to medication etc.
Ideally the follicles should grow at a rate of 1.64 +/- 0.02mm per day (9). Too slow or too fast beyond this rate show poorer results.
At this stage in IVF procedure they’ll also be looking at the uterus lining. In order to implant an embryo the lining needs to be about 6-8mm (though in some cases 17mm or more), and the blood needs to be triple-lined. Ideally I like my patients to present with a 9-10mm triple lining, as this shows greater implantation success (10, 11, 12) .
The final step in this stage is the trigger shot.
A woman is considered ready for egg retrieval when her follicles have reached 15-20mm in diameter (13, 14), that said various IVF fertility treatment clinics make up their own standard for this. Once she is good to go, the woman then injects a trigger shot containing Human Chorionic Gonadotrophin (hCG) of either 5000-10,000 IU into the muscle or under the skin or 250ug of recombinant hCG under the skin.
This is done 36 hours BEFORE egg retrieval and the timing here is VERY important. If the retrieval isn’t timed correctly after this trigger shot the follicles may rupture and the eggs suddenly released 38-40 hours after the shot.
IVF Fertility Procedure Continued...
So, we've covered the first two steps of IVF procedure. In the next article, we'll examine Step 3: Egg Retrieval, Step 4: Sperm Retrieval and Step 5: Insemination. Then in the final part in this series we'll look at Steps 6: Culture and Step 7: Transfer. Following that, we'l examine, what can go wrong in IVF and how to fix it and the side effects of IVF drugs, testing, and the other issues surrounding IVF procedure.
- Click here to go to part 2 and learn about Egg Retrieval, Sperm Retrieval and Insemination.
- Click here to go to part 3 and learn about Culture and IVF Transfers.
- Click here to learn about the Risks of IVF.
- Click here to discover the side effects of IVF.
In the meantime, if you want to get ALL the information you need Before IVF, check out my complete guide on the topic; "Before IVF: How it works, why it doesn’t and what you can do to Ensure Your IVF Success!". Over 430 pages, this guide provides answers to every question you could ask about fertility and reproductive health Before you go through IVF. Including a detailed walk through of the complete IVF procedure, all the medications, side effects and what you can do to make it work!
What's Your Next Best Step With IVF?
If you’re trying for a family or planning on going through IVF, ICSI IUI, or have been through failed rounds, from poor egg growth, fertilization failure, sperm quality issues, miscarriage etc, and want to give this round the best possible shot of success and dramatically improve your fertility and reproductive health, to have a happy healthy baby, then …
- Download my Free "9 Reasons You Can't Get Pregnant" Guide to learn more about what complications may be present and what you can do to fix them!
- Subscribe to my newsletter to keep up to date with the new articles, how to guides, fertility recipes and more.
- Get Your Copy of "Before IVF: How it works, why it doesn’t and what you can do to Ensure Your IVF Success!". Over 430 pages, this guide provides answers to every question you could ask about fertility and how to maximise your reproductive health. It will help you beat the numbers in IVF and better still may help you conceive without ever having to go through IVF!
- Contact me with your particular questions and concerns and I'll do my best to help. :-)
Footnotes
1. Sullivan EA, Zegers-Hochschild F, Mansour R, et al. International committee for monitoring assisted reproductive technologies (ICMART) world report: assisted reproductive technology 2004. Hum Reprod 2013;28:1375-90.
2. Sunkara SK, Coomarasamy A, Khalaf Y, et al. A three-arm randomised controlled trial comparing Gonadotrophin Releasing Hormone (GnRH) agonist long regimen versus GnRH agonist short regimen versus GnRH antagonist regimen in women with a history of poor ovarian response undergoing in vitro fertilisation (IVF) treatment: Poor :responders intervention trial (PRINT). Reprod Health 2007;4:12
3. MD04 female infertility pharmacotherapy - stimulation protocols. ASRM elearning course notes; 2010
4. http://www.independent.ie/irish-news/ivf-death-was-preventable-according-to-hse-report-26307110.html retrieved 5/9/17 29
5. Bosh E. Can we skip weekends in GnRH antagonist cycles without compromising the final outcome? Fertil Steril 2012;97:1299-300.
6. Griesinger G, Kolibianakis EM, Ventis C, et al. Oral contraceptive pretreatment reduces ongoing pregnancy likelihood on gonadotropin-releasing hormone antagonist cycles: an updated meta-analysis. Fertil Steril 2010;94:2382-4.
7. Van Wely M, Kwan I, Burt AL, et al. Recombinant versus urinary gonadotrophin for ovarian stimulation in assisted reproductive technology cycles. Cochrane Database Sys Rev 2011;(2):CD005354
8. Ji J, Liu Y, Tong XH, Luo L, Ma J, Chen Z. The optimum number of oocytes in IVF treatment: an analysis of 2455 cycles in China. Hum Reprod. 2013;28(10):2728-34.
9. Baerwald AR, Walker RA, Pierson RA. Growth rates of ovarian follicles during normal menstrual cycles, orla contraception cycles, and ovarian stimulation cycles. Fertil Steril 2009;91:440-9
10. Richter KS, Bugge KR, Bromer JG, et al. Relationship between endometrial thickness and embryo implantation, based on 1,294 cycles of in vitro fertilization with transfer of two blastocyst-stage embryos. Fertil Steril 2007;87:53-9.
11. Kovacs P, Matyas S, Boda K, et al. the effect on endometrial thickness on IVF/ICSI outcome. Hum Rerpod 2003;18:2337-41.
12. El-Toukhy T, Coomarasamy A, Khairy M, et al. The relationship between endometrial thickness and outcome of medicated frozen embryo replacement cycles. Fertil Steril 2008;89:832-9.
13. Blok L, Kremer J. In vitro fertilization and intracytoplasmic sperm injection. In: de Hann N, Spelt M, Gobel R, editors. Reproductive medicine: a textbook for paramedics. Amsterdam: Elsevier Gezondheidszorg; 2010. P. 105-26 [chapter 3].
14. MDO24 female infertility pharmacotherapy - stimulation protocols. ASRM elearning course notes; 2010.



New! Comments
Have your say about what you just read! Leave me a comment in the box below.